What is Value-Based Service (VBS)?
The healthcare industry is undergoing a seismic shift from the traditional fee-for-service approach to a Value-Based Service (VBS) model. This shift is being driven by a number of factors, including the Affordable Care Act, CMS plans, and regulations, alongside the need for more predictable and sustainable revenue streams.
Healthcare has long operated based on a practice of paying for each visit and procedure, but now several hospitals and insurers are experimenting with “pay-for-quality” models that compensate healthcare providers on how well they perform based on a set of criteria. Not only could this compensate doctors for better patient outcomes, but it will also encourage them to work together to reduce medical errors. This monumental change will bring about a new era of accountability and reliability in healthcare provision.
Revenue Model in VBS
The revenue model in VBS is based on the concept of “shared savings” between providers and health plans. Under VAC, health plans pay providers a set fee for a particular service or procedure. If the provider can deliver the service more efficiently or at a lower cost than expected, they will receive a portion of the savings back from the health plan. This incentivizes providers to reduce costs while still providing quality care, resulting in improved patient outcomes and reduced costs for both parties. This type of system has several advantages over the traditional fee-for-service model, such as improved patient outcomes, greater efficiency, and increased cost savings.
Accountable Care Organization (ACO)
Single specialty providers or individual specialists coalesce to form an Accountable Care Organization (ACO) under the CMS Medicare Shared savings program (MSSP), aiming to provide efficient and comprehensive care to their patients. These organizations safeguard people from preventable illnesses and illness progression through routine coordinated care.
ACO works on two revenue models based on risk-taking capabilities, each with its own unpredictable outcome. If providers deliver the expected care or reach the set benchmark in the Upside model, they are rewarded with financial incentives from the insurer but will not be held financially liable for falling short. Meanwhile, the Downside (Two-sided) Risk Model offers a riskier bet where providers can gain greater rewards – but with a risk of potentially incurring greater losses in the form of a portion payment if expectations are not met. Basically, the value-based healthcare revenue model is a risk-sharing arrangement between a payer and a provider.
Bundled Payment
The bundled payment model, more commonly referred to as the Episode Payment Model, is a lump sum payment made by the payer that is intended to cover each of the predetermined episodes of care. If costs exceed the estimated price, the payer will reduce the payment amount, while if costs are lower than the estimated price, the savings are shared amongst all participants in the system. This binding agreement pushes providers to become more efficient, as their profits depend on them controlling costs within this dynamic system.
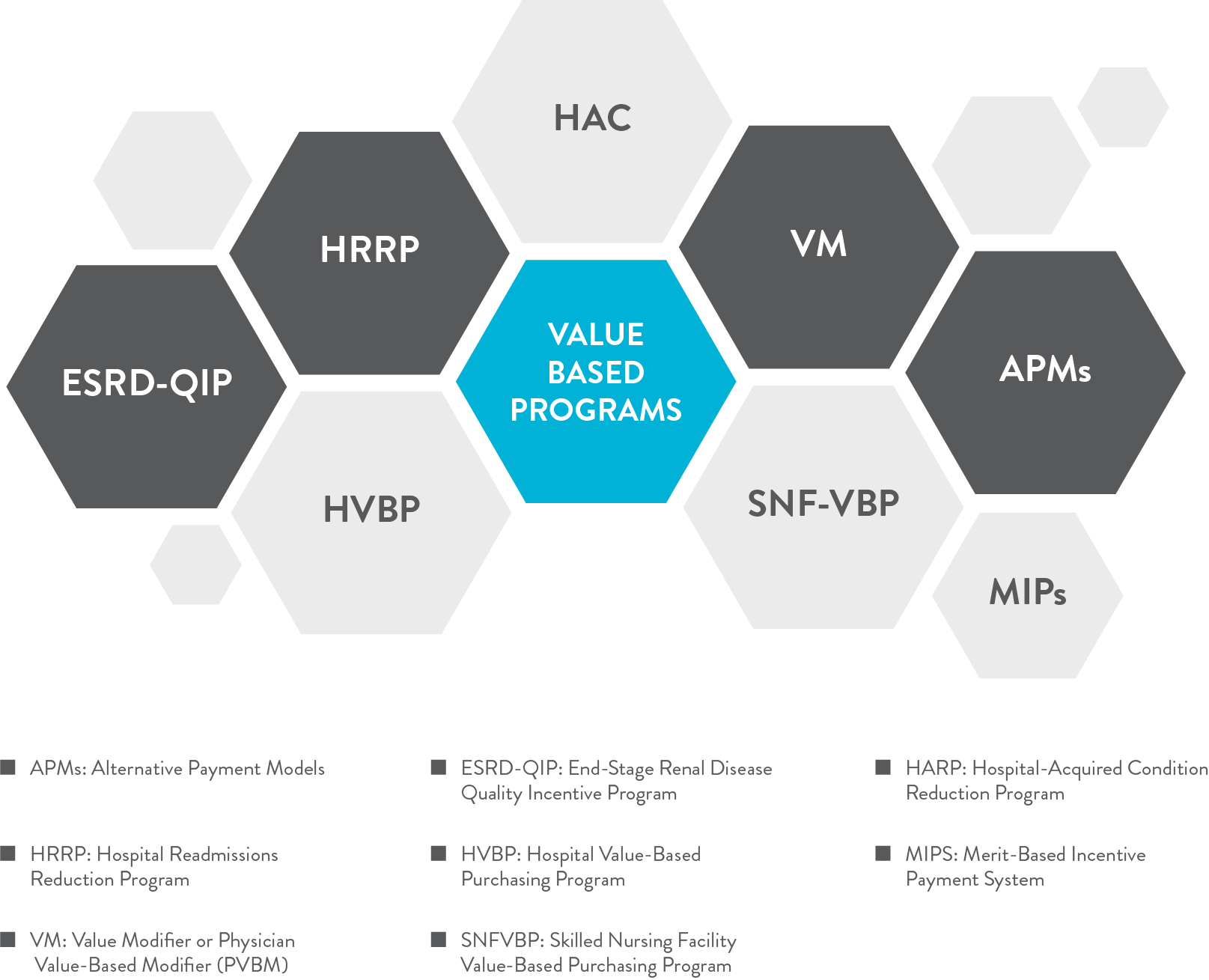
CMS has designed various innovative value-based programs with a fluctuating risk-to-reward ratio, all in the cause of accountable care. By leveraging these revolutionary programs, providers can access newfound financial and clinical rewards while still delivering high-quality care.
Benefits of a Value-Based Healthcare Revenue Model
The value-based healthcare revenue model has a number of benefits. The VBS model incentivizes providers for keeping costs within a set budget and achieving quality metrics. This is beneficial for both the payers and providers since it encourages collaboration to contain costs, and improve quality by eliminating unnecessary procedures or services. All parties have better visibility into quality and cost metrics. This builds trust between all the stakeholders which ultimately reduces claim denials. Bundled payment help reduces the administrative burden associated with billing and reimbursement, allowing providers to focus on providing quality care. By sharing risk and potential financial rewards, both payers and providers have a common goal of the patient’s health and well-being. It also entices providers to focus on preventive risk management and invest in technology and human resources that can help them better manage patient health and better returns.
How to Implement a Value-Based Healthcare Revenue Model?

Most value-based healthcare revenue models are implemented on a larger scale and involve collaboration between multiple stakeholders. Before jumping in and implementing a value-based model, it’s important to assess the impact it will have on your organization. This includes evaluating how you will go about achieving the objectives of the model, measuring performance, and ensuring compliance. Once you have determined that the model is right for you, the next step is to build a cross-functional team to drive the implementation. This team should include executives, clinicians, financial and operational leaders, and data analysts apart from physicians and providers. Their responsibility will be to evaluate existing processes, identify gaps and areas of improvement, and develop strategies to fill those gaps. The team also needs to be up-to-date on the latest technology and have an understanding of data analytics, which can help in predictive MDM (Medical Decision Making) with better accuracy. They should also have an understanding of the regulations and plans mandated by CMS, as well as any potential benefits or risks that might arise from the implementation of the model.
Tips for Success
There are several tips and strategies to keep in mind in order to ensure success with a value-based healthcare revenue model.
- In the VBS, it is critical to devise strategies that improve quality while keeping costs in check. Evidence-based medicine and protocols, patient-centered care, and better coordination between providers are essential elements in ensuring that every service rendered yields optimal value. Having a clearly defined set of goals and objectives for the model, as well as measurable outcomes that can be measured and tracked for both quality and cost objectives, can maximize the chances of success.
- Population health management plans must be used to mitigate risks and costs associated with the VBS. Stratification, disease management, preventive care tactics, and data analysis can help to identify those at risk of developing a medical condition and act before the situation worsens. By implementing these strategies into the system, providers can reduce the risk associated with VBS and garner more savings.
- Data analytics is a critical component of any value-based healthcare revenue model. Investing in data analytics can be a game changer in predictive modeling, as it ensures that all data points are accurate and up-to-date. Without accurate data, it would also be very difficult to measure progress and make necessary adjustments as needed.
- Continuously evaluate and refine processes and systems. This includes staying up-to-date on changes in technology, regulations, and industry trends. Building relationships and proactive collaboration with other stakeholders is also important.
- Finally, set up a team structure that can support the objectives of the VBS model, as well as develop and implement training so that stakeholders are well-versed in the model.
Conclusion
The value-Based Healthcare Revenue Model is the revolutionary solution that propels all stakeholders in the system – insurers, patients, hospitals, and physicians – toward a common goal: delivering optimum care for the patient. By diligently strategizing and focusing on quality, providers can experience benefits, such as streamlined operations, slashed costs, and superior quality of care. Indeed, it’s an advantageous collaboration for all involved.
Check your business’s current RCM model and risk-bearing capacity to choose the best suitable VBS program. Book a call with our expert to get a free audit of your practice. We will navigate you in all steps to understand the arcane and achieve the best out of it with our best practices and strategies from experts.
OR click on our website https://cosentus.com/ to know more about us and our bundled MedXP service.

